Photo Competition
Photographs of patients, pathology specimens, Gram stains, EKGs, and radiographic studies or other visual data may be submitted. Your submission should depict clear examples of findings that are relevant to the practice of emergency medicine or findings of unusual interest that have educational value. If your submission is accepted, you must mount it for viewing.
No more than three different photos may be submitted for any one case.
Submissions for the AAEM18 Photo Competition are now closed.
Submission Instructions
Photo submissions must be accompanied by a brief case history and case discussion, written as an “unknown.”
The case history is limited to no more than 250 words and should include:
- Chief complaint
- History of present illness
- Pertinent physical exam (other than what is depicted in the photo)
- Pertinent laboratory data
- One or two questions asking the viewer to identify the diagnosis or pertinent finding.
The case discussion should be brief (ideally no more than 750 words) and must be submitted in a separate MS Word document. The case discussion should include the following information:
- Answer(s) and brief discussion of the case, including an explanation of the findings in the photo
- One to three bulleted take home points or “pearls.”
Please submit only blind copies, omitting your name, institution, city, state, or any other identifier.
Photo Submission Guidelines
The case history is limited to no more than 250 words. If accepted for display, AAEM reserves the right to edit the submitted case history and discussion. Submissions are selected based on educational merit, relevance to emergency medicine, quality of the photograph, the case history, and appropriateness for public display. If your photograph is accepted, you will be notified and informed of set-up and dismantle times. Patients and patient identifiers must be appropriately masked. Additionally, you must attest that written consent and release of responsibility have been obtained for all photos EXCEPT for isolated diagnostic studies such as EKGs, radiographs, Gram stains, etc.
Responsibility for bringing photo and case submission(s) to the Scientific Assembly rests with the submitter. A 3.5´ x 3.5´ square area will be available for each submission. Photo competition participants who submit by 11:59pm CST on November 27, 2017, will receive notification of acceptance or rejection by January 29, 2018.
Presenting Author Information
Only one individual may submit a photo through the online submission portal. If your submission is accepted for display at Scientific Assembly, you may include the names of co-authors and co-submitters on the display.
Previous Presentations of Photos
Any photo that has been previously published or used in a national conference competition should not be submitted. Photos that have been presented at international meetings (MEMC) and have not been published, can be submitted for consideration.
Sample Photo Submission
Chelsea Dymond, MD

Chief Complaint:
Facial pain and congestion: Not just sinusitis.
History of Present Illness:
A 39 year old female with a past medical history of hypertension presents to the Emergency Department (ED) complaining of left-side facial and neck pain for one week with associated symptoms of congestion, left eyelid swelling and mild blurred vision. She states that she saw her primary care doctor two days prior and was diagnosed with a sinus infection for which she was prescribed over-the-counter decongestants and she would now like you to prescribe her antibiotics. She denies any recent trauma.
Physical Exam:
VITALS: BP: 146/90, Pulse: 68, Temp: 98.6, RR: 18, SpO2: 100% on room air
GENERAL: No distress, well appearing female
NEURO: Alert and oriented, normal strength (5/5) all extremities, normal sensation
CRANIAL NERVES: SEE PHOTO
HEENT: Left facial tenderness over the maxillary sinus, left neck tenderness under the mandible and mild nasal congestion
RESPIRATORY: Breath sounds clear and equal bilaterally
CV: Normal S1 S2 with no added sounds, regular rhythm, no murmurs, rubs or gallops
ABDOMEN: Soft non-tender, non-distended
SKIN: Warm and dry with no evident rash
Questions:
- What physical exam finding is noted in the photo?
- What are the not-to-be-missed causes for this finding?
Answers:
- Partial Horner syndrome with signs of subtle left eye ptosis, miosis, but no anhidrosis
- Spontaneous carotid artery dissection
Case Discussion:
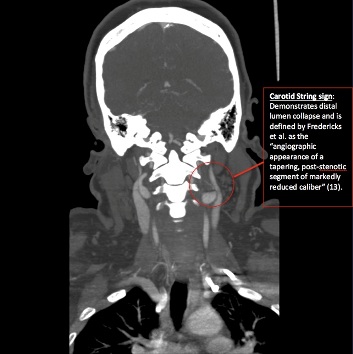
Given her history and physical exam, a computed tomography angiogram (CTA) head and neck was ordered with concern for carotid artery dissection. Chemistry and complete blood count was within normal limits and chest x-ray was unremarkable. CTA head was negative for any acute intracranial process. CTA neck revealed a high-grade stenosis of the left internal carotid artery with a string sign up until the level of the foramen lacerum with subsequent complete occlusion. Vascular neurology was consulted and she was admitted for management of left internal carotid artery dissection with resulting partial Horner syndrome. Subsequent brain MRI was negative for infarct. She was started on aspirin and clopidogrel for stroke prevention and atenolol for hypertension. She noticed mild improvement in her ptosis and blurred vision and was discharged the following day with vascular neurology following as an outpatient.
Internal carotid dissection occurs when a small intimal tear allows high-pressure arterial blood to enter the artery wall and dissect between the blood vessel layers leading to intramural hematoma, aneurysmal dilation or vessel occlusion. High-risk consequences include microemboli leading to a high rate of associated stroke, specifically in young persons less than 50, and mass effect on the surrounding structures (1). Extracranial dissections are more common than intracranial, with the most common location being 2cm above the bifurcation of the common carotid artery (1). Risk factors include blunt or penetrating trauma, connective tissue disorders, hypertension, migraine with aura and smoking.
While carotid artery dissection is rare, with an incidence of only 3 per 100000, the rate has been steadily growing due to advancing imaging in recent years (3). Early presentation includes subtle signs of headache and neck pain and is most often preceded by head or neck trauma (1). However, in one study of 126 patients, approximately one third presented with a partial Horner syndrome. Partial Horner syndrome is caused by either ischemic changes or compression of the sympathetic chain that runs along the internal carotid artery. Anhidrosis does not occur due to sweat gland innervation traveling along the external carotid artery (3).
Ischemic stroke has been shown to occur in up to 86% of all dissections and is responsible for 20% of strokes in the younger adult population, giving the need for a high index of suspicion among EM physicians (2). However, this diagnosis can easily be missed in the ED given a reasonable workup for new-onset headache and neck pain is a non-contrast computed tomography (CT) scan and possible lumbar puncture. A non-contrast CT is likely to miss an uncomplicated dissection (1, 4). A CTA and magnetic resonance angiography (MRA) are the gold standard for diagnosis.
Given the high incidence of stroke, patients presenting with acute ischemic stroke should be evaluated and treated with intravenous thrombolytics when indicated. Studies have shown that there is no difference in outcome even if carotid artery dissection is ultimately identified (2, 5, 12).
Once carotid artery dissection is diagnosed, management centers on administering antiplatelet therapy or anticoagulation for prevention of stroke. There has been long debate over appropriate treatment with multiple meta-analyses showing no therapeutic benefit between using anticoagulation or antiplatelet therapy (5, 9, 10). The recent CADISS trial released in April 2015 was the first randomized prospective trial comparing the two therapy arms and showed no difference in outcome between them. In the past anticoagulation has often been preferred for its assumed action of preventing recurrent embolus from the site of dissection, however in theory it could increase the risk of local hematoma extension, further exacerbating stenosis and leading to hemodynamic compromise (5). After the release of the CADISS trial it has been suggested that due to the greater safety profile of antiplatelet therapy it may become first choice for patients with acute carotid artery dissection (7). Additionally, recent literature has proposed that endovascular stent-assisted thrombolysis for occlusion secondary to internal carotid artery dissection is a safe and promising treatment modality (8,11).
In conclusion, EM physicians should recognize the risk factors and presentation of carotid artery dissection and maintain a high index of suspicion for the subtle signs and symptoms that warrant further investigation.
Pearls:
- A painful, partial Horner syndrome can present as a sign of carotid artery dissection
- Patient perceptions can be misleading, and recognizing subtle physical findings will help guide you to the correct diagnosis
If you have questions regarding submissions, please call AAEM at (800) 884-2236 or email Rebecca Sommer at rsommer@aaem.org.


