COVID-19 - Trying Not to Intubate Early & Why ARDSnet may be the Wrong Ventilator Paradigm
Additional Resources from REBEL EM:
Hey there REBEL Cast listeners, Salim Rezaie here. For me and I am sure many COVID-19 has been quite the whirlwind. So much information, so little time to process all of it. Meanwhile, many of us are on the frontlines having to take care of these patients. Personally, I have never been so wrong, so many times about a single disease process. What I say today, may be different tomorrow. This podcast was recorded on April 3rd, 2020 so any information that comes out after this, might change the viewpoints that are expressed today.
Special Guests:
David A. Farcy, MD FAAEM FACEP FCCM
President of the American Academy of Emergency Medicine
Chairman, Department of Emergency Medicine
Director, Emergency Medicine Critical Care
Mount Sinai Medical Center in Miami Beach, FL
Twitter: @DFarcy
Evie Marcolini, MD FAAEM FACEP FCCM
Associate Professor of Emergency Medicine and Neurocritical Care
Geisel School of Medicine at Dartmouth, Hanover, New Hampshire
Board of Directors, American Academy of Emergency Medicine
Twitter: @EvieMarcolini
Cameron Kyle-Sidell, MD
Critical Care Medicine
Emergency Medicine
Maimonides Medical Center
Brooklyn, NY
Twitter: @cameronks
Ashika Jain, MD, RDMS, FACEP, FAAEM
Associate Professor
Trauma Critical Care
Emergency Ultrasound
Ronald O Perelman Department of Emergency Medicine
New York University/Bellevue Hospital Center, NY
Twitter: @4shikajain
This podcast is longer than we typically do on REBEL Cast (1hr 30min), however there is lots of information that is critical in the treatment of COVID-19 patients with pneumonia. The questions we tackled were as follows:
- Many of us have been working under the paradigm that COVID-19 PNA eventually develops into ARDS in the sickest patients. It appears to me that these patients don’t fit into this paradigm. Many have normal to high compliance and there are certainly reports of patients not showing any signs of distress. What are you seeing clinically?
- One of the big fears with using NIV/HFNC is aerosolization. This is a real risk, but for many we are in full PPE which should make this risk minimal. What are your thoughts on NIV/HFNC as an intermediary step for some patients in terms of staff safety and the patients in front of us?
- In my reading of available evidence, patients with COVID-19 PNA who get intubated have a mortality rate of anywhere from 50 – 90%. Many studies reporting in the 80% range. This is not a causation of intubation and mechanical ventilation but an association as most of these reports are observational and retrospective. In other words, maybe the patients were just so sick they were going to have a high mortality anyways. On the flip side this higher mortality may also be the fact that we are intubating patients early and using the ARDSnet protocol. What are you currently using to manage patients on the ventilator?
- In my mind patients present into one of 4 clinical categories and I want to go over these one at a time…
- Suspected or confirmed COVID-19 with minimal symptoms. These patients can most likely go home, but one big concern is how do we follow them up. What are you using to decide who can go home and who can’t? How are you following them up?
- Silent Hypoxemia (“Happy Hypoxemia”): These patients often have low O2 sats but have no external signs of respiratory distress, AMS, or lack of perfusion. In my mind these patients are prime candidates for NIV/HFNC and awake proning. Are any of you using awake proning? Any logistical issues with this?
- Intermediate Hypoxemia: These patients often have low O2 sats but have some mild symptoms of respiratory distress such as tachypnea and tachycardia. These patients may require intubation but may also benefit from NIV/HFNC + Awake proning. What is your threshold to consider intubation?
- Respiratory Distress: These patients require intubation and are too far gone in my opinion to test NIV/HFNC. Many of these patients will have high pulmonary compliance with hypoxic vasoconstriction in the lungs. It seems increasing PEEP and prone positioning may be of minimal help with recruitment of collapsed lungs (i.e ARDSnet). High PEEP (>15cmH20) may also compromise cardiac filling. What ventilation strategies do you recommend in these patients with the limited information we have thus far?
- Suspected or confirmed COVID-19 with minimal symptoms. These patients can most likely go home, but one big concern is how do we follow them up. What are you using to decide who can go home and who can’t? How are you following them up?
- One concern I have heard is that patients not intubated can crash quickly. It might be too risky to not intubate early. Is there a good way to predict this or what are you doing to mitigate this?
- Evie I would like to ask you a few questions specifically in regard to neurological concerns:
- How are you handling patients with stroke symptoms and suspected COVID-19. Imaging, systemic thrombolysis, endovascular therapy?
- There appear to be lots of reports of headache and AMS as a common symptom. I am unaware of CSF studies to date, but should we be concerned about encephalitis? Do these patients need LPs?
- Do we have any idea about the mechanism or prognosis of these patients?
- What are your final take home messages for the listeners to remember?
References:
- ARDS Definition Task Force. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA 2012. PMID: 22797452
- Grasso S et al. ARDSnet Ventilatory Protocol and Alveolar Hyperinflation: Role of Positive End-Expiratory Pressure. Am J Resp Crit Care Med 2007. PMID: 17656676
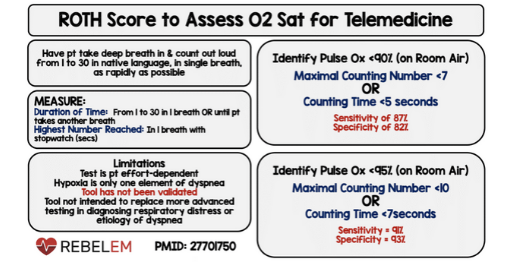
- Chorin E et al. Assessment of Respiratory Distress by the Roth Score. Clin Cardiol 2016. PMID: 27701750
- Gattinoni L. Prelimiary Observations on the Ventilatory Management of ICU COVID-19 Patients. SFAR 2020. [Epub Ahead of Print]
- Gattinoni L et al. COVID-19 Does not Lead to a “Typical” Acute Respiratory Distress Syndrome. ATS 2020. [Epub Ahead of Print]
For More on This Topic Checkout:
REBELEM: COVID-19 Hypoxemia - A Better and Still Safe Way
