Summer 2020
Welcome from EUS-AAEM
The Emergency Ultrasound Section of the American Academy of Emergency Medicine (EUS-AAEM) is founded to foster the professional development of its members and to educate them regarding point-of-care ultrasound. This group will serve as a venue for collaboration among medical students, residents and practitioners who are interested in point-of-care ultrasound. The purpose of our group is to augment the knowledge and expertise of all emergency medicine specialists and to advocate for patient safety and quality care by endorsing bedside ultrasound. Membership is not limited to fellowship trained physicians. All emergency medicine practitioners passionate about ultrasound are welcome to join and participate.
We are proud to publish our e-newsletter with original contributions from many of our members. We encourage all members to submit for future editions. Topics include but are not limited to educational, community focus, interesting cases, resident and student section, and adventures abroad.
For more information visit us online at: www.aaem.org/EUS.
In this Issue:
-
President's Message
-
Ultrasound Building Blocks: Lung Ultrasound in the COVID-19 Pandemic
-
Resident Section: Calculating Left Ventricular Ejection Fraction using End Point Septal Separation
-
Ultrasound Highlights: Pediatric Intussusception
-
Fellow Section: Anterior Shoulder Dislocations: Radiographs or Point-of-Care Ultrasound?
-
US Guided Procedures: Ultrasound-guided Aspiration of Olecranon Bursitis
-
Administrative Corner: PAs and POCUS in Emergency Medicine
-
Ultrasound Saves: Pump Up Your POCUS Skills
-
From Journal to Practice: Starting an Ultrasound Journal Club
-
Letter to the Editors
-
Get Involved
President's Message
Hello EUS-AAEM Members,
I am excited to serve as the EUS-AAEM President for 2020-21. First, I want to thank Dr. Eric Chin for leading us this past year. I hope to continue to build on his great work and provide value to our members.
Things have certainly changed since last year, as COVID-19 has impacted our professional and personal lives in a number of ways. Over the past year, we successfully launched our first regional ultrasound course and developed a skills verification program for emergency physicians no longer in training. While these will both be on hold during this pandemic, we would hope to resume these again in the future when it is safer to hold in-person workshops.
In the interim, we plan to work hard on your behalf to advocate for emergency ultrasound and will be utilizing the newsletter to share knowledge and resources amongst the membership. In this issue, we will be discussing a variety of topics including musculoskeletal applications, intussusception, lung ultrasound in COVID-19 patients, and more.
There are many ways to get involved with EUS-AAEM. Please reach out if you would like to learn more.
Sincerely,
Michael Gottlieb, MD FAAEM
EUS-AAEM President 2020-21
Ultrasound Building Blocks
Lung Ultrasound in the COVID-19 Pandemic
Shawn Sethi, DO
PGY-3 Emergency Medicine
Einstein Healthcare Network - Philadelphia, PA
The COVID-19 outbreak began December of 2019 in Wuhan, China and has since become a global pandemic. Patients may present with a characteristic viral pneumonia on chest x-ray and ground-glass opacities on chest CT imaging. As the pandemic has grown there has been significant discussion regarding alternative imaging modalities for these patients. Recently we’ve seen an emergence of preliminary literature regarding the use of bedside lung ultrasound for evaluation of viral pneumonia from the SARS-CoV-2 virus.
A report from the European Review of Medical Pharmacology presented the case of a 52-year-old male with signs and symptoms typical of COVID-19, including multiple high-risk exposures, who eventually tested positive for the virus.1 The patient presented with shortness of breath and was found to be hypoxic to 90% on room air. His lung examination was remarkable for bilateral crackles and his chest x-ray showed perihilar opacities. He subsequently underwent bedside lung ultrasound by the emergency provider. These providers used a wireless curvilinear probe connected via Bluetooth to a tablet. The emergency physician scanned while a nurse held the tablet and performed functions including recording and storing clips. Both the ultrasound probe and tablet were kept in sterile bags and changed after each patient encounter. The authors describe a 12-zone technique including anterior, lateral and superior areas with both superior and inferior segments in each.
They found several characteristic features on bedside lung ultrasound including irregular pleural lines, subpleural consolidations, and thick, confluent B-lines. These findings were compared to a control group patient with similar symptoms, but who was found to be COVID-19 negative, which showed normal pleural lines and thin, regular and infrequent B-lines. The authors note that these abnormal findings likely represent interstitial alveolar damage. Authors from another study, a retrospective analysis of 20 patients with SARS-CoV-2 infection, found similar abnormalities on lung ultrasound in addition to findings of poor blood flow to areas of consolidation.2 See lung ultrasound clips below regarding these characteristic findings.
Figure 1. Visualization of irregular pleural line3
Figure 2. Visualization of confluent B-lines4
There has been significant discussion in the medical community regarding using chest CT as a “screening tool” for COVID-19. A case series from the diagnostic radiology literature found chest CT to have a sensitivity of 98% compared to the sensitivity of viral PCR for SARS-CoV-2 at 71%.5 However, there are many disadvantages to CT including ionizing radiation, increased cost and length of stay in the ED. Traditionally, ultrasound has shown several advantages compared to other imaging modalities such as CT, including portability, non-invasive nature and the ability to easily perform serial examinations. Specifically, in the setting of the COVID-19 pandemic, bedside ultrasound provides further advantages compared to chest CT including exposing less providers to the patient (i.e. nursing, radiology technologists) and the ease of sterilization of the ultrasound probe compared to a CT suite. In addition, the CT findings of SARS-CoV-2 tend to occur later in the disease course, which could lead to false negative results. Lung ultrasound also provides an advantage compared to auscultation with a stethoscope, given the ability of the provider to maintain more distance from the patient and lessening the chance of droplet transmission.
In light of the COVID-19 pandemic, emergency medicine providers need to consider the risks and benefits to imaging studies performed on those with suspected infection. Given the significant advantages compared to more traditional modalities, lung ultrasound should be considered in those with concern for COVID-19.
References
- Buonsenso, D et al. Point-of-Care Lung Ultrasound findings in novel coronavirus disease-19 pnemoniae: a case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020 Mar;24(5):2776-2780. doi:10.26355/eurrev_202003_20549.
- Huang, Y et al. A Preliminary Study on the Ultrasonic Manifestations of Peripulmonary Lesions of Non-Critical Novel Coronavirus Pneumonia (COVID-19). [PrePrint]. Feb 26 2020. doi:10.21203/rs.2.24369/v1
- Macias, Michael et al. "Pleural Findings in COVID-19." The POCUS Atlas. 7 April 2020. http://www.thepocusatlas.com/covid19. Accessed 12 May 2020.
- Macias, Michael et al. "Confluent B Lines." The POCUS Atlas. 7 April 2020. http://www.thepocusatlas.com/covid19. Accessed 12 May 2020.
- Fang Y et al. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. Feb 19 2020:200432. doi:10.1148/radiol.2020200432. [Epub ahead of print]
Resident Section
Calculating Left Ventricular Ejection Fraction using End Point Septal Separation
Andrea Sarchi, DO and Melissa Myers, MD FAAEM
Case Presentation
A 76-year-old female with past medical history of hypertension and hyperlipidemia presents with exertional shortness of breath over the last week. Vital signs are notable for a heart rate of 110 and blood pressure of 162/96 mm Hg. Temperature, respiratory rate, and oxygen saturation are all within normal limits. Physical exam is notable for an elderly female in mild respiratory distress with tachycardia but is otherwise unremarkable. EKG is normal. At this point, you are most concerned for congestive heart failure and pulmonary embolism but aren’t sure which diagnostic workup to pursue. You decide to use point-of-care ultrasound to narrow the differential.
Discussion
Bedside echocardiography can be a valuable tool in the emergency physician’s workup of chest pain, shortness of breath, hypotension, cardiac arrest, and trauma.1 Early determination of LVEF, presence of pericardial effusion and evaluation for right ventricular dilation can quickly direct Emergency Physicians towards the correct diagnosis.
There are multiple ways to measure LVEF including the “eyeball” technique, fractional shortening, Simpson’s Method, and EPSS.2 The “eyeball” technique, as the name implies, involves a visual estimation of LVEF by looking at the difference in left ventricular size between systole and diastole. Most cardiologists utilize this approach and it is extremely accurate to the trained eye.3 However, many emergency department providers have not analyzed hundreds of echocardiograms and could thus benefit from a more objective approach.3
The fractional shortening method involves the anterior-posterior measurement of the left ventricular dimension to estimate LVEF. It is the least accurate method and prone to errors in patients with coronary artery disease and wall motion abnormalities.2,3 The Simpson’s Method of Discs gives the most accurate estimation of LVEF. However, it is rarely used in the emergency department as it is time consuming and requires the cardiac package on the ultrasound machine.2 Finally, EPSS is a commonly used technique that provides a quick and effective means for estimating LVEF.2,3
The utility of end point septal separation in estimating LVEF was first demonstrated in a 1977 study in The American Journal of Cardiology. It showed a high negative correlation (r = -.86) between end point septal separation and angiographic LVEF.4 A study of 108 patients in 1983 showed that an EPSS greater than 7 mm had a sensitivity of 87% and specificity of 75% in detecting individuals with angiographically reduced LVEF less than 50%.5 In 2006, a study comparing LVEF based on end point septal separation with that based on magnetic resonance imaging found that LVEF could be calculated using the following formula: LVEF = 75.5 – 2.5 (EPSS in mm).6 Finally, a study in 2011 demonstrated a high correlation between measurements of LVEF by EPSS performed by resident emergency physicians with visual estimations of LVEF by senior emergency physicians and cardiologists.7
EPSS is evaluated using a parasternal long axis window showing good visualization of the mitral valve (MV). Once this window is obtained, place the machine into motion mode (M-mode) and put the cursor line through the tip of the MV (Figure 1). Identify the E waves (early diastolic filling) and A waves (atrial contraction) on the screen, and measure the distance from the tip of the E wave to the septum (Figure 2).2 This value is your end point septal separation. Using the formula from the 2006 study discussed above, an EPSS < 5 mm correlates with a normal LVEF, an EPSS >7 mm correlates with a LVEF <50%, and an EPSS>18 mm correlates with a LVEF <30%.3,6 In the case presented, the patient’s EPSS was 3.8 mm. This is < 5 mm and thus normal. Specifically, when using the formula for LVEF, the patient’s ejection fraction is 75.5 – 2.5(3.8) = 66%. This is within normal limits.
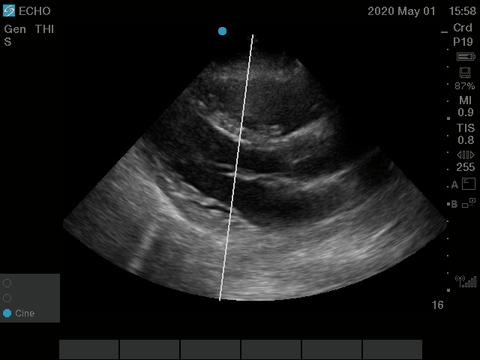
Figure 1. Parasternal long axis view with M-mode line through the tip of the anterior leaflet of the mitral valve.
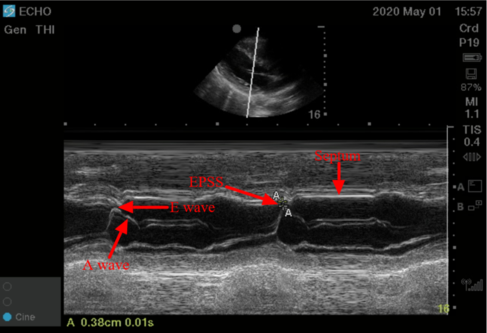
Figure 2. M-mode tracing showing the septum, E waves, and measurement of EPSS.
Limitations
Conditions that can falsely elevate the EPSS include mitral stenosis/Rheumatic Heart Disease, mitral calcification, and aortic insufficiency.2,3 In mitral stenosis and mitral calcification, there is decreased excursion of the MV anterior leaflet and thus an elevated EPSS.2,3 In aortic insufficiency, the regurgitant blood flow can push down the MV anterior leaflet and cause an elevated EPSS despite a normal LVEF.2,3 Therefore, if a patient has any of these conditions, an alternative method for estimating LVEF should be pursued.
If you have a patient with atrial fibrillation, there will be no A-wave. Studies have also shown that EPSS may be variable in different beats in a patient with atrial fibrillation and it is suggested that you average 3-5 measurements for the most accurate EF measurement.8
Conclusion
Point-of-care cardiac ultrasound is a valuable tool to the emergency provider that allows for rapid evaluation of patients with chest pain, dyspnea, hypotension, trauma, and cardiac arrest.1 EPSS is a quick, objective method for emergency providers to obtain an estimated LVEF that correlates highly with the eyeball technique performed by cardiologists and experienced emergency providers.2-7 EPSS is another ultrasound technique that can lead to improved patient care and utilization of resources.
Case Conclusion
You decide to do a point-of-care cardiac ultrasound and you measure an end point septal separation of 3.8 mm, indicating a normal ejection fraction. You proceed to order a computed tomography pulmonary angiogram which shows a right segmental pulmonary embolism. Heparin is started and the patient is admitted to medicine.
The views expressed herein are those of the authors and do not reflect the official policy or position of the Brooke Army Medical Center, the U.S. Army Medical Department, The U.S. Army Office of the Surgeon General, the Department of the Army, the Department of the Air Force, or the Department of Defense, or the U.S. Government.
References
- Arntfield RT, Millington SJ. Point of care cardiac ultrasound applications in the emergency department and intensive care unit - a review. Curr Cardiol Rev. 2012;8(2):98–108. doi:10.2174/157340312801784952
- Mallin M, Dawson M. Chapter 1. Echocardiographic Assessment of Cardiac Output and Ejection Fraction. Introduction to Bedside Ultrasound: Volume 2. Lexington, KY: Emergency Ultrasound Solutions; 2013. https://books.apple.com/us/book/introduction-to-bedside-ultrasound-volume-2/id647356692. Accessed May 1, 2020.
- Mallin M, Dawson M. Episode 25 – EPSS + App Release. UltrasoundPodcast.com. 2012. Available at: http://www.ultrasoundpodcast.com/tag/epss/. Accessed May 1, 2020.
- Massie BM, Schiller NB, Ratshin RA, Parmley WW. Mitral-septal separation: new echocardiographic index of left ventricular function. Am J Cadio. 1977;39(7):1008-1016. doi:https://doi.org/10.1016/S0002-9149(77)80215-4
- Ahmadpour H, Shah AA, Allen JW, Edmiston WA, Kim SJ, Haywood LJ. Mitral E point separation: a reliable index of left ventricular performance in coronary artery disease. Am Heart J. 1983;106(1):21-28. doi:10.1016/0002-8703(83)90433-7
- Silverstein JR, Laffely NH, Rifkin RD. Quantitative estimation of left ventricular ejection fraction from mitral valve E-point to septal separation and comparison to magnetic resonance imaging. Am J Cardiol. 2006;97(1):137-140. doi:10.1016/j.amjcard.2005.07.118
- Secko MA, Lazar JM, Salciccioli LA, Stone MB. Can junior emergency physicians use E-point septal separation to accurately estimate left ventricular function in acutely dyspneic patients? Acad Emerg Med. 2011;18(11)1223-1226. doi:10.1111/j.1553-2712.2011.01196.x
- Lehmann KG, Johnson AD, Goldberger AL. Mitral valve E point-septal separation as an index of left ventricular function with valvular heart disease. Chest. 1983;83(1):102â€108. doi:10.1378/chest.83.1.102
Ultrasound Highlights
Pediatric Intussusception
Aleksandr Gleyzer, MD FAAEM; Jennifer Chao, MD; and Isaac Gordon, MD
A 19-month-old male was brought by his parents to the emergency department due to eight episodes of vomiting since morning. Parents denied fever, rash, diarrhea, bloody or black stools, cough, rhinorrhea, or any other symptoms. On exam, patient was awake, but looked tired with an intermittent weak cry. He was afebrile, vitals stable. His abdomen was soft, nontender, with no organomegaly or masses. Rest of exam was unremarkable. Plain abdominal X-ray was obtained that showed a soft tissue density in the right upper quadrant with a lack of the air in the ascending colon concerning for intussusception (Figure 1). Abdominal ultrasound showed a classical target sign that confirmed the diagnosis of intussusception (Figure 2). Patient was transferred to another institution with a pediatric surgery service.
Vomiting is a common chief complaint in the pediatric emergency department. Although in most cases it is due to a self-limited viral illness, a clinician must maintain a high degree of suspicion for intussusception. Abdominal X-ray might show a mass and a lack of air in the ascending colon that raises suspicion of the disease. However, an unremarkable X-ray should not stop the work up. The mean sensitivity of the X-ray was reported as 80.5% and the mean specificity as 58%.1 Therefore, clinician should proceed to the ultrasound that has a reported sensitivity of 98.4% (95% CI, 95.2%-100.0%) and specificity of 96.4% (95% CI, 94.0%-98.9%). It has a negative predictive value 99.5% (95% CI, 98.6%-100.4).2 The classical target sign on the abdominal ultrasound will confirm the diagnosis.
References
- 1. Smith DS, Bonadio WA, Losek JD, Walsh-Kelly CM, Hennes HM, Glaeser PW, Melzer-Lange M, Rimm AA. The role of abdominal x-rays in the diagnosis and management of intussusception. Pediatr Emerg Care. 1992 Dec;8(6):325-7.
- 2. Henderson AA, Anupindi SA, Servaes S, Markowitz RI, Aronson PL, McLoughlin RJ. Comparison of 2view abdominal radiographs with ultrasound in children with suspected intussusception. Pediatr Emerg Care. 2013 Feb;29(2):145-50.
Figure Legend
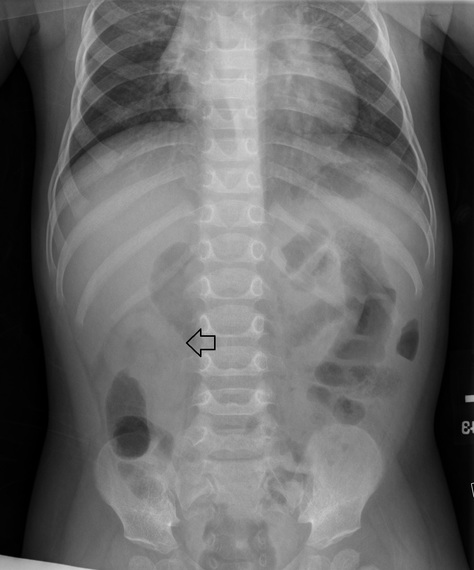
Figure 1. Plain abdominal X-Ray image showing right upper quadrant mass (black arrow).
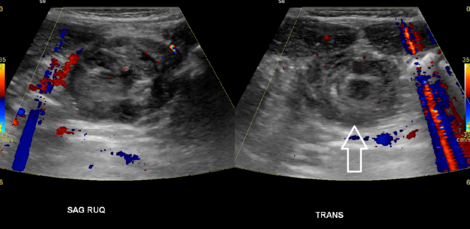
Figure 2. Transverse and Sagittal abdominal ultrasound images showing soft tissue mass including a classical “target sign” (white arrow).
Fellow Section
Anterior Shoulder Dislocations: Radiographs or Point-of-Care Ultrasound?
Waroot Nimjareansuk, DO; Robert Farrow, DO; and Michael Rosselli, MD
Case Description
A 29-year-old male with a history of multiple right shoulder dislocations presented to the emergency department with right shoulder pain, swelling, and deformity immediately after throwing a football. His vitals were within normal limits. His physical examination showed a right shoulder deformity with significantly decreased range of motion. His distal sensation and pulses were intact with normal capillary refill. Emergency department (ED) point-of-care ultrasound (POCUS) of the right shoulder showed an anterior dislocation of the right shoulder as seen in Figure 1. This image demonstrates an anterior dislocation in a single posterior glenohumeral view.
To obtain these ultrasound images, the patient was placed in a sitting position with the ultrasound operator standing behind the affected shoulder and the ultrasound screen in front of the patient. A low-frequency curvilinear transducer was placed at the posterior aspect of the shoulder below the scapular spine in transverse position with probe marker to the patient’s left. The transducer was scanned out laterally toward the humerus while adjusting the depth until the glenoid and the head of the humerus came into view. An anterior dislocation was shown with the head of the humerus deep to the screen and the glenoid closer to the probe.
Discussion
Anterior shoulder dislocations are a common complaint to the ED. Traditionally, pre-reduction radiographs and post-reduction radiographs are obtained. Pre-reduction radiographs have the potential to delay treatment and are unlikely to change emergency department management for patients with atraumatic recurrent shoulder dislocations.1-2 This suggests that there may be a role for POCUS in the management of shoulder reductions in the ED.
The use of POCUS for the evaluation of shoulder dislocations in the ED has been shown to not only accurately detect dislocation, but also can confirm successful reduction.3 A systematic review of 306 patients in seven studies showed that POCUS was 99.1% sensitive and 99.9% specific for the diagnosis of shoulder dislocation with no statistically significant difference when compared to plain radiography.3 One study showed 100% sensitivity in both the ultrasound detection of shoulder dislocations and the assessment of complete reduction of the shoulder joint.4 POCUS is not only accurate in diagnosing shoulder dislocations and reductions, but it also takes significantly less time than radiography.5 An additional benefit of using ultrasound (US) with cases of shoulder dislocation is that if the physician chooses to use procedural sedation for the reduction, a quick POCUS study can be utilized immediately after reduction attempt to confirm a successful reduction at bedside before the patient has recovered from the sedation.6
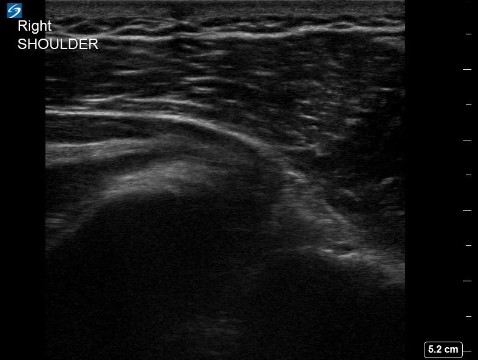
Figure 1. Pre-reduction ultrasound of the right shoulder showing an anteriorly dislocated humeral head in relation to the glenoid. Posterior Glenohumeral View.

Figure 2. Post-reduction ultrasound of the right shoulder showing the relocated shoulder. Posterior Glenohumeral View.
Case Conclusion
An intra-articular hematoma block with lidocaine was performed under US guidance utilizing an in-line technique and the same posterior glenohumeral view as was used to confirm dislocation. After analgesia was achieved via the hematoma block the dislocated shoulder was successfully reduced with external rotation. The shoulder reduction was then confirmed at bedside on POCUS as shown in Figure 2. The patient was subsequently placed in a sling and swathe and given instructions to follow up with orthopedic surgery as an outpatient. This case demonstrates the utility of the posterior glenohumeral view on US to evaluate and care for anterior shoulder dislocations. When coupled with a range of analgesic options such as intra-articular and brachial plexus blocks there is a potential for US to impact the current management of patients presenting to the ED with shoulder dislocations.
References
- Abbasi S, Molaie H, Hafezimoghadam P, Zare MA, Abbasi M, Rezai M, Farsi D. Diagnostic Accuracy of Ultrasonographic Examination in the Management of Shoulder Dislocation in the Emergency Department. Ann Emerg Med. 2013;62(2):170-75.
- Hendey GW. Necessity of Radiographs in the Emergency Department Management of Shoulder Dislocations. Ann Emerg Med. 2000;36(2);108-13.
- Gottlieb M, Hollad ay D, Peska GD. Point-of-care ultrasound for the diagnosis of the shoulder dislocation: A systematic review and meta-analysis. Am J Emerg Med. 2019;37(4):757-61.
- Shuster M, Abu-Laban RB, Boyd J. Prereduction Radiographs in Clinically Evident Anterior Shoulder Dislocations. Am J Emerg Med. 1999;17(7):653-58.
- Seyedhosseini J, Saiidian J, Taheri AM, Vahidi E. Accuracy of point-of-care ultrasound using low frequency curvilinear transducer in the diagnosis of shoulder dislocation and confirmation of appropriate reduction. Turk J Emerg Med. 2017;17(4):132-35.
- Halberg MJ, Sweeney TW, Owens WB. Bedside ultrasound for verification of shoulder reduction. Am J Emerg Med. 2009;27(1):134.e5-6.
US Guided Procedures
Ultrasound-guided Aspiration of Olecranon Bursitis
Waroot Nimjareansuk, DO and Michael Rosselli, MD
Mt Sinai Medical Center Miami Beach
Case
60-year-old male presents with right elbow pain and swelling for one month. Patient denies any other symptoms. He had normal vital signs in ED, including being afebrile. His olecranon bursa was tense and fluctuant with minimal tenderness to palpation and no pain on full range of motion or associated erythema or warmth. Ultrasound of the olecranon bursa showed a septated bursa filled with anechoic fluid between the olecranon process and the skin. Patient was anesthetized with lidocaine and ultrasound-guided aspiration was performed producing 10 ml of serosanguinous fluid. No fluid analysis was performed as there was low clinical suspicion for septic bursitis.
Olecranon bursitis is a relatively common complaint to the emergency room. It is most frequently caused by minor trauma such as chronic leaning and or repetitive elbow motion although major trauma, rheumatoid arthritis, gout, lupus, and uremia should also be considered.1 While most causes of olecranon bursitis are aseptic, the olecranon bursa is the most common site of septic bursitis. For the majority of cases, the bursa is nontender and the elbow joint has painless full range of motion. Conservative therapy for olecranon bursitis consists of PRICE, NSAIDs, and bursal aspiration. Intrabursal methylprednisolone acetate can also be used in conjunction with aspiration,2 although repeat steroid injections should be avoided due to risk of triceps rupture.3
Aspiration of olecranon bursitis is often safe and effective. In one systematic review of 29 studies containing 1,278 patients, the risk of bursal infection did not increase with aspiration of aseptic bursitis.4 In another literature review, bursal aspiration has been shown to relieve pain and discomfort due to the pressure of the distended bursa.5,6 In addition, ultrasound-guided aspiration is useful to ensure the entirety of the bursal fluid is drained and identifies the structure/content of the bursa, possibly detecting underlying abscesses, loose bodies, rheumatoid nodules, or gout tophi.7 A consensus statement by the American Medical Society for Sports Medicine supports that ultrasound-guided interventions of the elbow are accurate with one study showing 100% accuracy of elbow joint ultrasound-guided injections.
Procedure
- Create a sterile field, including ultrasound probe with sterile cover and sterile gel.
- Place a high-frequency linear probe at the olecranon bursa longitudinally using an in-plane approach parallel to the forearm with indicator towards the site of aspiration.8 Fluid at the olecranon bursa should appear as an anechoic area between the skin and the olecranon process.
- Use an 18 or 20 gauge needle on a 10 ml syringe and direct the needle along the same parallel line as the forearm. Advance the needle and aspirate withdrawing the fluid. In most instances, the aspirate will have the appearance of a blood-tinged serous fluid. If there is concern for septic bursitis, fluid analysis can be sent to the laboratory. Apply a bandage or ace wrap around the elbow to help prevent recurrence.1,9
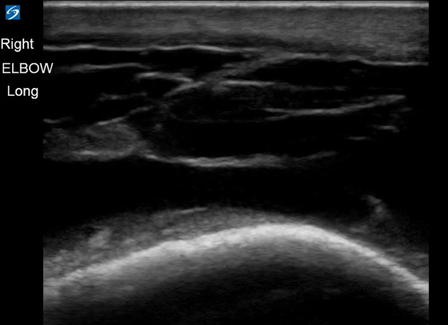
Figure 1. Anechoic fluid at olecranon bursa visualized under ultrasound
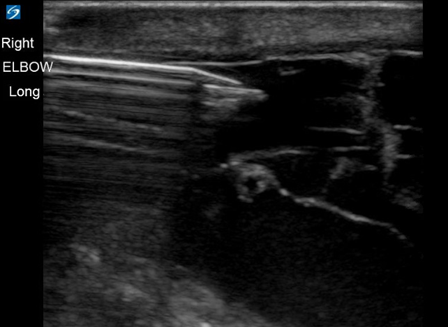
Figure 2. Ultrasound-guided aspiration of olecranon bursa
References
- Roberts J, Hedges J, editors. Clinical Procedures in Emergency Medicine. 7th ed. Chapter 52: Treatment of Bursitis, Tendinitis, and Trigger Points. pp 1086-1089. Philadelphia, PA: Elsevier, Inc; 2018.
- Lockman L. Treating nonseptic olecranon bursitis: a 3-step technique. Can Fam Physician. 2010. 56(11):1157.
- Stannard JP, Bucknell AL. Rupture of the triceps tendon associated with steroid injections. Am J Sports Med. 1993;21(3):482.
- Sayegh ET, Strauch RJ. Treatment of olecranon bursitis: a systematic review. Arch Orthop Trauma Surg. 2014;134(11):1517-36.
- Baumbach SF, Lobo CM, Badyine I, Mutschler W, Kanz KG. Prepatellar and olecranon bursitis: literature review and development of a treatment algorithm. Arch Orthop Trauma Surg. 2014;134(3): 359-70.
- Sorani A, Campbell R. Image-guided elbow interventions: a literature review of interventional treatment options. Br J Radiol. 2016;89(1057):20150368.
- Blankstein A, Ganel A, Givon U, Mirovski Y, Chechick A. Ultrasonographic findings in patients with olecranon bursitis. Ultraschall Med. 2006;27(6):568-71.
- Peck E. Outpatient Ultrasound-Guided Musculoskeletal Techniques, An Issue of Physical Medicine and Rehabilitation Clinics of North America. E-Book Volume 27, Issue 3 of The Clinics: Orthopedics. Elsevier Health Sciences, 2016.
- Smith DL, McAfee JH, Lucas LM, Kumar KL, and Romney DM. Septic and nonseptic olecranon bursitis. Utility of the surface temperature probe in the early differentiation of septic and nonseptic cases. Arch Intern Med 1989;149(7):1581-85.
- Del Buono A, Franceschi F, Palumbo A, Denaro V, Maffulli N. Diagnosis and management of olecranon bursitis. Surgeon. 2012;10(5):297-300.
Administrative Corner
PAs and POCUS in Emergency Medicine
Amie Billstrom, PA-C MMS and Kerri Van Arnem, DSc EMPA
Physician Assistants (PAs) have been incorporated into emergency departments (EDs) since the early 1970s, preceding the establishment of emergency medicine (EM) as a specialty by the American Board of Medical Specialties.1 Currently, over 12,000 PAs work in EM, which is approximately 13% of all certified PAs.2 Between 2010 and 2017, an estimated one billion US emergency department (ED) visits occurred, with 5.0% of visits seen by a PA, and 8.2% by a PA and EM physician team.3 Therefore, PAs contribute, on average, to approximately 16.5 million ED patient encounters annually.
To date, there is significant disagreement among emergency physicians (EPs) as to the appropriate scope of practice for PAs in the ED setting. The consensus by both the American College of Emergency Physicians (ACEP) and American Academy of Emergency Medicine (AAEM) is that PAs should not practice independently or unsupervised in the ED, but instead be a member of an EP-lead team.4,5 This team approach is advocated for by our EP partners to protect the patient. The emergency department is a high stakes environment, where patients present with a variety of complaints, with unpredictable levels of acuity, that in the most emergent cases, require immediate life-saving interventions. Board-certified EM physicians receive 15,000-16,000 supervised clinical hours in their residency, compared to the 2,000 hours physician assistants receive during their undergraduate medical training.6,7 PAs working in EDs require the support and mentorship of their EM physician colleagues to provide the additional education and training required to be successful in this field. Currently, 80% of PAs that work in EM cite on-the-job training, provided primarily by EPs, as the source of their education in advanced EM diagnostics and procedures, to include point-of-care ultrasound (POCUS).8
In recognition of ultrasound as a “skill integral to the practice of emergency medicine” and to ensure EP competency, in 2007, the Accreditation Council for Graduate Medical Education (ACGME) added diagnostic and procedural ultrasound as milestones to the EM residency curriculum, requiring all EM residents to perform a minimum 150-300 proctored, high quality POCUS studies prior to graduation. In order to attain clinical competence, the ACEP ultrasound guidelines from 2016, recommends EPs achieve 25-50 quality reviewed POCUS exams in each of the 12 EM core applications: trauma, intrauterine pregnancy, abdominal aortic aneurysm (AAA), cardiac/hemodynamic assessment, biliary, urinary tract, deep vein thrombosis, soft tissue/musculoskeletal, thoracic/airway, ocular, bowel, and procedural guidance.9
POCUS performed in EM, also known as Emergency ultrasound (EUS), requires fundamental knowledge of exam indications, image acquisition, image interpretation, and integration of the findings into patient management.10,11 Given this, POCUS is a bedside diagnostic tool, not a specialized physical exam skill like a slit lamp exam, nor is it a procedure, like a fracture reduction, which are more easily taught, real-time, at the bedside while caring for patients. POCUS is an operator-dependent clinical adjunct, that requires an intensive didactic component, as well as repetitive hands-on training, which is not easily obtained during a busy ED shift. Despite no formal didactic POCUS training for PAs, one survey reports 27% of PAs are currently using ultrasound in their clinical practice, although this data was not limited to those practicing in the ED.12 Because the scope of practice of PAs so individualized, dependent on the state government, medical institution, and supervising physician, it is unclear whether quality assurance is being performed on these studies and whether they are being performed independently. Additionally, according to the 2009 Report on Emergency Medicine Physician Assistants, approximately 15% of EMPAs work 50% or more of their shifts without on-site EP supervision, while an additional 7% work without any EP supervision at all, despite the EM physician objections.13 With this and the aforementioned report that approximately 1 in 4 PAs currently use POCUS in their practice, should we be alarmed as a profession that we may be using a powerful diagnostic tool to direct patient care without the recommended training or credentialing?
As mentioned, PAs working in emergency medicine rely heavily on on-the-job (OTJ) training and are not required to complete a formal postgraduate residency in EM prior to being hired in an ED. Despite this, ACEP has published a policy statement that encourages PA training in ultrasound using the same competency guidelines required by EPs, but does not provide a recommended training pathway for Pas.14 In 2017, the Society of Emergency Medicine Physician Assistants (SEMPA) issued a statement that PAs should receive privileges in POCUS when they have met the same training standards as their EM physician colleagues. This implies following one of two pathways, via residency training or practice based training, as laid out by ACEP.15 Given only 15% of EMPAs have attended a formal EM residency, performing 150 high quality scans, that are proctored and provided quality assurance by an ultrasound expert, while on the job, without any formal academic or training system in place, is a daunting task for even the most experienced and motivated PA in EM.
Because POCUS is an EM residency curriculum milestone, most graduating EM physicians will have met the credentials set forth by ACEP for privileging in POCUS prior to graduation. Many residency programs recognize the importance of the didactic portion regarding POCUS, to include quality assurance sessions and review of ultrasound literature, therefore have dedicated academic time or rotations to EUS. Additionally, medical school leadership in the U.S. has included 90 core clinical ultrasound milestones in their didactics to prepare future physicians to utilize POCUS in their residency training.16 In contrast, it is estimated only 12% of PA schools include ultrasound training, didactic or clinical, in their curriculum and as of the January 2019 Content Blueprint for the Physician Assistant National Certifying Examination (PANCE), performance or interpretation of bedside ultrasound is not listed. 17,18 Additionally, of the PA EM residencies, only 67% include a POCUS curriculum, given ultrasound has not yet been identified as a milestone for EMPA training.8
As PAs in EM, how can we best learn the essential components of EUS using a practice based or OTJ training model? There is currently no suggested or approved practice-based POCUS curriculum sanctioned by our professional governing bodies such as SEMPA, the American Academy of Physician Assistants (AAPA), the Physician Assistant Education Association (PAEA), or the National Commission on Certification of Physician Assistants (NCCPA). Ideally, this practice-based training model would be evidenced based, parallel the didactics utilized in medical schools, and EM residencies, and provide hand-on training recommendations that are feasible in multiple EM practice settings. PA POCUS education, training and eventual privileging should not be limited to those PAs who attend post-graduate programs or work within the infrastructure of an academic setting that has ultrasound dedicated EP faculty willing to train them.
Though PA education is anchored in its adherence to the medical model, EMPAs are not physicians and do not receive the specialty training that our EP leaders have. However, we are at the bedside, just as our physician colleagues, and if the standard for PA privileging in POCUS is going to be the same as our EP counterparts, as stated by ACEP and SEMPA, we ought to advocate for a standard curriculum to obtain comparable ultrasound training. The training model will need to look different, given our professional development is rooted in on-the-job training, and our scope of practice is subject to many more factors that are not considered for physicians. Collectively, we will also need to brainstorm and address training recourse to a multitude of scenarios such as if a PA works in an ED that does not have ultrasound dedicated faculty or one that does not have the ability to archive POCUS studies, nor conducts internal quality assurance. We would also need to provide training solutions for the PA whose veteran supervising EP is not privileged in POCUS, which may eliminate that PAs ability to receive the training through their institution all together. As a consequence, the EMPA practice-based POCUS training model may need innovation using telemedicine, hand-held ultrasound technology and asynchronous self-directed learning. Regardless, there are solutions. However, it is essential that this training curriculum be standardized, vetted as well as endorsed by our PA organizational leadership, so that all PAs have the ability to complete the training, obtain the credentials and then advocate for their POCUS privileges at their respective institutions. Both PAs and POCUS have demonstrated their contributions to emergency medicine individually, now we need to demonstrate our value together.
The views expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army, the Department of the Air Force, the Department of Defense, or the U.S Government.
References
- Kraus CK, Carlisle TE, Carney DM. Emergency medicine physician assistant (EMPA) postgraduate training programs: Program characteristics and training curricula. West J Emerg Med. 2018. doi:10.5811/westjem.2018.6.37892
- National Certification of Physician Assistants Commission I. 2016 Statistical Profile of Certified Physician Assistants An Annual Report of the National Commission on Certification of Physician Assistants Message from the President/CEO.; 2016.
- Wu F, Darracq MA. Physician assistant utilization in U.S. emergency departments; 2010 to 2017. Am J Emerg Med. 2020. doi:10.1016/j.ajem.2020.02.009
- American College of Emergency Physicians. Guidelines Regarding the Role of Physician Assistants and Advanced Practice Registered Nurses in the Emergency Department. Policy Statement. https://www.acep.org/patient-care/policy-statements/guidelines-regarding-the-role-of-physician-assistants-and-advanced-practice-registered-nurses-in-the-emergency-department/. Published 2013. Accessed May 1, 2020.
- American Academy of Emergency Medicine. Updated Position Statement on Advanced Practice Providers. Position Statement. https://www.aaem.org/resources/statements/position/updated-advanced-practice-providers. Published 2019. Accessed May 1, 2020.
- Farcy DA. Taking a Stand on the Independent Practice of APPs. American Academy of Emergency Medicine. https://www.aaem.org/resources/publications/common-sense/issues/presidents-message/taking-a-stand-on-the-independent-practice-of-apps. Published 2020. Accessed May 3, 2020.
- American Academy of Physician Assistants. PA Education-Preparation for Excellence. https://www.aapa.org/wp-content/uploads/2016/12/Issue_Brief_PA_Education.pdf. Published 2019. Accessed May 4, 2020.
- Society of Emergency Medicine Physician Assistants. EMPA Education Data. 2009 Report on Emergency Medicine Physician Assistants. htts://www.sempa.org/practice-management/empa-education-data/. Published 2009. Accessed May 3, 2020.
- American College of Emergency Physicians. Ultrasound Guidelines: Emergency, Point-of-care, and Clinical Ultrasound Guidelines in Medicine. Policy Statement. https://www.acep.org/patient-care/policy-statements/ultrasound-guidelines-emergency-point-of--care-and-clinical-ultrasound-guidelines-in-medicine/. Published 2016. Accessed May 2, 2020.
- The Society of Point of Care Ultrasound. POCUS Practice Guidelines. Practice Guideline. https://spocus.org/admin-resources/practice-guidelines/. Published 2018. Accessed May 2, 2020.
- Monti J. Revolution or evolution? A proposal for the integration of point-of-care ultrasound into physician assistant clinical practice. J Physician Assist Educ. 2017. doi:10.1097/JPA.0000000000000101
- Rizzolo D, Krackov R. PA use of point-of-care ultrasound: A pilot survey. J Am Acad Physician Assist. 2018. doi:10.1097/01.JAA.0000533668.18568.e9
- Society of Emergency Medicine Physician Assistants. Clinical Practice Data. 2009 Report on Emergency Medicine Physican Assistants. https://www.sempa.org/practice-management/clinical-practice-data/. Published 2009. Accessed May 5, 2020.
- American College of Emergency Physicians. Advanced Practice Provider Point-of-Care Ultrasound Guidelines. Policy Statement. https://www.acep.org/globalassets/new-pdfs/policy-statements/advanced-practice-provider-point-of-care-ultrasound-guidelines.pdf. Published 2019. Accessed May 2, 2020.
- Society of Emergency Medicine Physician Assistants. Statement on Ultrasound Guidelines on Credentialing and Privileging. https://www.sempa.org/globalassets/sempa/media/pdf/professional-development/sempa-endorsement-of-acep-us-guidelines-on-credentialing-and-privileging.pdf. Published 2018. Accessed May 5, 2020.
- Dinh VA, Lakoff D, Hess J, et al. Medical student core clinical ultrasound milestones: A consensus among directors in the United States. J Ultrasound Med. 2016. doi:10.7863/ultra.15.07080
- Rizzolo D, Krackov RE. Integration of Ultrasound Into the Physician Assistant Curriculum. J Physician Assist Educ. 2019. doi:10.1097/JPA.0000000000000251
- National Commission on Certification of Physician Assistants. Content Blueprint for the Physician Assistant National Certifying Examination (PANCE). PANCE Content Blueprint. https://www.nccpa.net/pance-content-blueprint. Published 2019. Accessed May 5, 2020.
Ultrasound Saves
Pump Up Your POCUS Skills
Nicole Del Valle, MD and Maninder Singh, MD
Case Presentation
A 50-year-old male with a history of hypertension, diabetes and alcohol abuse was brought in by EMS after being involved in a motor vehicle accident. The patient was the restrained driver when he crashed into a highway divider. He admitted to drinking alcohol and states that the airbags deployed. EMS reported front-end damage to the car but an ambulatory patient on arrival. Upon arrival, the patient’s vital signs revealed a heart rate of 110, blood pressure of 143/92 and a fingerstick glucose of 102. Physical exam was significant for alcohol on breath. The rest of the physical exam was unremarkable and the patient denied any pain or other complaints. The bladder portion of the FAST exam is shown below (Figure 1). What is the diagnosis?
Case Discussion
The bladder images revealed a fluid collection on the left side of the bladder (Figure 2). Given that the patient had experienced trauma and was tachycardic, there was an initial concern this could be a positive FAST exam. However, upon further questioning, the patient admitted to having a penile implant, explaining this “fluid collection” and the balloon inside this collection (Figure 3).
Erectile dysfunction affects more than 50 million American men each year. Fortunately, this problem can be solved with a penile implant. Inflatable penile implants account for more than 90% of all penile prosthesis. This type of prosthesis consists of three parts: (1) a small pump implanted in the scrotum that, when squeezed, causes fluid to flow from a (2) reservoir in the pelvis to (3) two cylinders in the penis (Figure 4). Although urologists are very familiar with penile prosthesis, it is important for emergency department physicians to recognize the cystic structure of the prosthesis reservoir on ultrasound and its relationship to the bladder. Failure to do so can lead to a misdiagnosis (i.e. free fluid in pelvis in the setting of trauma) and unnecessary procedures or further imaging on the patient.
Questions
- What is the most serious complication of a penile implant?
- Rupture
- Infection
- Malfunction
- Hematuria
- Anuria
- When does infection of a penile prosthesis usually occur?
- within 7 days post implant
- within 2 weeks post implant
- within 3 months post implant
- within 5 months post implant
- What is the most common organism involved in penile implant infections?
- Escheri coli
- Staphylococcus aureus
- Staphylococcus epidermidis
- Streptococcus agalactie
- Staphylococcus epidermidis and Streptococcus agalactie
Answers
- Infection. Explanation: Infection is the most fearsome and serious complication of a penile implant. If left untreated, it can lead to deep tissue necrosis and if very severe, may even require penile amputation.
- Within 3 months. Explanation: Infection after penile prosthesis insertion usually occurs within 3 months post-op.
- Staphylococcus epidermidis and Streptococcus agalactie. Explanation: Staphylococcus epidermidis or Streptococcus agalactie are the most common cause of infection of penile implants; more rarely, toxic bacteria like Escherichia coli, Staphylococcus aureus, Enterococcus faecalis cause infection earlier in the post-op course and are more severe.
References
- Bettocchi, C et al. “Penile prosthesis: what should we do about complications?.” Advances in urology vol. 2008 (2008): 573560. doi:10.1155/2008/573560
- Lazarou, S. Surgical Treatment of Erectile Dysfunction. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA
- Quinn, M et al. “Sonographic Appearance of An Inflatable Penile Prosthesis.” J. Ultrasound Med. 4:567- 569, October 1985
- Aydin, M et al. “Current Surgical Management of Erectile Dysfunction.” Journal of Academic Research in Medicine, vol. 1, no. 2, 2012, pp. 61–64., doi:10.5152/jarem.2011.17.
Figures
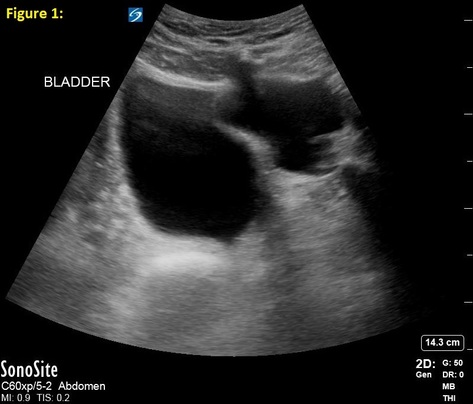
Figure 1
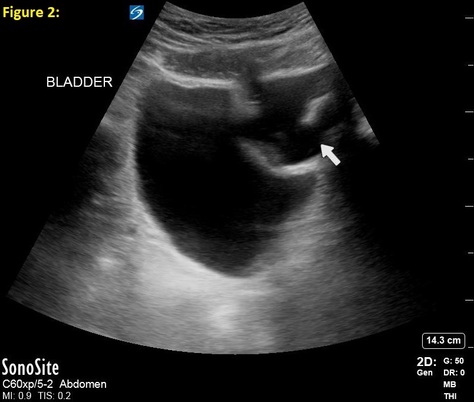
Figure 2

Figure 3
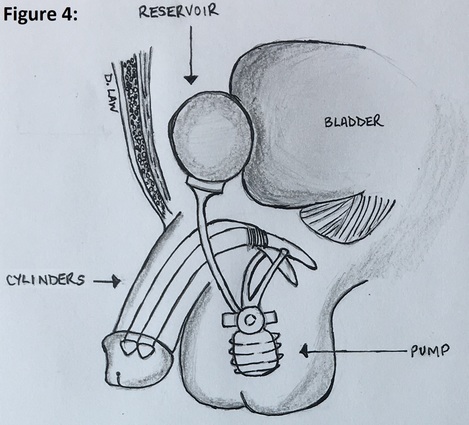
Figure 4 (Image designed by Doris Law, PA)
Supplementary GIFs
Supplementary 1: Longitudinal view of the bladder during the FAST exam
Supplementary 2: Transverse view of the bladder during the FAST exam
From Journal to Practice
Starting an Ultrasound Journal Club
Shawn Sethi, DO
PGY-3 Emergency Medicine
Einstein Healthcare Network - Philadelphia, PA
An important aspect of ultrasound education involves evidence based medicine (EBM). One of the ways in which EBM can be incorporated into an emergency ultrasound division is by holding regular ultrasound journal clubs to review landmark and novel ultrasound related literature. Our residency started an ultrasound journal club last year which meets regularly, here are some take-aways for starting one at your own residency:
Why start?
Appraising and staying up-to-date with medical literature is an essential skill for physician trainees. However, a 2010 survey of 98 emergency medicine (EM) educators found that only 25% reported formal journal clubs or EBM curricula.1 Another survey of 64 EM programs found that only 22% taught more than five hours of EBM content per year.2 As bedside ultrasound has become fully incorporated into emergency medicine training programs, it is important to ensure understanding of the literature. Some ultrasound divisions provide opportunities to attend journal clubs for those on an ultrasound rotation. However, this may leave residents having to seek out literature on their own. Having a regularly scheduled journal club allows for a longitudinal learning experience that covers a variety of topics.
How to start?
An important step to starting a journal club is to identify faculty champions within your emergency department or ultrasound division. Although our institution is a large academic center with an emergency ultrasound division, one can find such attendings familiar with ultrasound at smaller community sites. Our ultrasound journal club is resident run with strong faculty support and provides credit towards asynchronous learning for those in attendance.
How to schedule meetings?
We hold meetings every other month with rotating topics of discussion. We find this schedule frequent enough to cover a large range of topics, while not too frequent as to overwhelm participants from joining. Typically, these occurred at venues capable of accommodating 10-20 people. However, in light of the recent pandemic we have transitioned to virtual video conferencing for the journal club. This allows for distinct advantages including the ability to share both still images (e.g. figures from articles) and movies (e.g. ultrasound clips). Effort is made to leave significant time for discussion after the articles are presented.
How to pick topics?
We find it easiest to pick a theme for each session to narrow down article selection. We select one to two “landmark” articles to serve as a foundation with an additional “advanced” topic to promote further discussion of recent advancements in POCUS. So far we have covered topics including ultrasound for trauma, ocular complaints, pneumonia, and TTE/TEE for cardiac arrest among others. Articles are sent out ahead of time for review by attendees. It can be advantageous to incorporate free open access medical education resources such as podcasts or online article summaries into the journal club; this is especially helpful for those unable to attend.
How can it be expanded further?
After each ultrasound journal club we create article summaries to be published on our residency webpage. As the journal club expands there is significant opportunity to involve other departments both within your hospital and surrounding institutions. Given how ubiquitous ultrasound has become throughout other medical specialties, interdepartmental partnerships are possible with critical care, surgery, OBGYN, or orthopedics for example. We recently began interhospital collaboration with two nearby emergency ultrasound divisions. This allows for an exchange in perspectives between faculty and residents when it comes to the variety of ultrasound practice.
Creating an ultrasound journal club is a rewarding experience which can lead to improved resident education and foster collaboration both within your program and beyond.
Letter to the Editors
What stood out to you from this issue of the POCUS Report? Have a question, idea, or opinion? Alexis Salerno, MD FAAEM and Melissa Myers, MD FAAEM welcome your comments and suggestions. Submit a letter to the editor and continue the conversation here.
Get Involved
We encourage original submissions to this e-newsletter and to our recurring section in Common Sense. Please contact us with any questions at EUS@aaem.org. Stay Calm and Ultrasound On!
